Dental calculus
For the periodontal diseases:
- The primary etiologic factor is: Is the dental plaque.
- The associated factor: is the dental calculus, it helps in new formation of the plaque.
- The modifying factor: is a systemic disease, it aggravates the disease when the plaque is presents.
Calculus:
- Is a mineralized dental plaque that occurs in the tooth surfaces & dental prosthesis, it has many forms:
- Bridging over the gingival margin.
- Follow the festooning shape of the dentition.
- Lobular form.
- In case of malalignment :àprotected area for the plaque à calculus
Classification:
Supragingival & subgingival calculus..
Generally: both can occur together or one may appear alone.
Subgingival calculus:
- Gingival fluid origin.
- Below the crest of the gingival margin.
- Hard, dark& flint like.
- Greenish black or dark brown in color.
- Firmly attached to the tooth, can’t be seen and detected by explorer No.621 probe.
- Extent nearly to the base of the pocket in chronic periodntitis, but doesn’t reach the Junctional epithelium.
Supragingival calculus:
- Saliva origin.
- Coronal to the gingival margin. Can be composed of supra &sub gingival calculus.
- Hard, clay like consistency, White, white yellowish in color& its color may be affected by the tobacco or food stain.
- Easy to be seen in the oral cavity, may be generalized or localized.
- Easy to be removed &usually recurrent especially in the: Lower incisors.
- Most common location :near to the orifices of the S. glands’ ducts
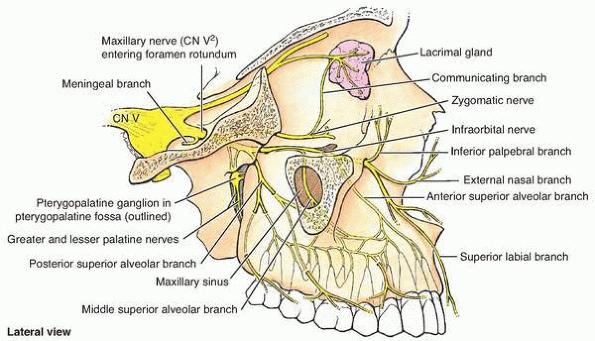
Parotid gland’s duct ”stenson”----->opposite to buccal surface of maxillary molars.
Submandibular “bartholine” & sublingual “wharton” ducts ----->Lingual surface of lower incisors.
it’s shape : either covers the occlusal surfaces or bridge like structure over interdental papilla.
Calculus contents:
Inorganic contents:70-90% | Organic contents | ||
2/3 of the calculus inorganic component is in crystalline form ;there are 4 types of crystals . The crystals are: hydroxyappatite ,58% à magnesium white locate,21% àmost in post octacalcium phosphate,12% Brushite, 9% àmost in mandibular anteriors. Detected more frequently in supragingival calculus. Constitute the bulk. Generally 2 or more crystals are detected in the calculus. Incidence of 4 crystals à varies with age of calculus. | Mixture of : Protein-poly saccharide complex + desquamated host cells (leukocytes & host cells) + microorganisms. Carbohydrates (1.9-9.1%): Glucose , glactose ,mannose ,arabinose ,rhamnose glucoric acid ,glactouric acid glucoseamine & glactose amine. à all are present in saliva except : Rhaminose & arabinose . Salivary proteins (5.9-8.2%): Most are amino acids. lipids 0.2%:nutral fat ,fatty acids ,cholesterol ester, phospholipids & cholesterol. | ||
*Contents: | The differences Supra gingival calculus | Between: Sub gingival calculus | |
hydroxyappatite: Ca Ph : Mg white: brushite: ratio of Ca/Ph: sodium contents: salivary proteins: | Equal. More. Less. More. Low. Increase with the depth of PD pocket. Yes | Equal Less. More Less. Higher. No. | |
Calculocementum:
Is the calculus has morphological appearance similar to cementum. This is because the calculus is interdigitates the cementum & no differences between them.
Mode of attachment of the calculus to the tooth surface:
- Close adaptation under surface depression.
- In sub gingival calculus.
- By organic pellicle (very weak)
- Penetration of the bacteria to the cementum.
- Mechanical interlocking to the surface irregularities: resorption lacuna or caries, in the cementum by sharpies fibers.
Calculus formation:
Calculus is the dental plaque that undergoes mineralization.
Calcification starts 4-8 hrs after plaque.
50 % become mineralized after 2 days.
60-90 12 days.
- Plaque can be daily removed at home by brushing but the calculus is
- not ,it is only removed clinically by the dentist .
- Calculus formation à the bacterial action will stopped (adv) but it will act as stagnation area for new plaque accumulationà (protection for plaque).
- Early plaque contains small amount of inorganic material but it will increase as the plaque develops into calculus.
- All plaque doesn’t necessarily undergo calcification.
- It reaches a plateau of maximal mineral by 2 days.
- Microorganisms are not always essential in calculus formation.
- Plaque has ability to conc. The Ca at 2-20 times it’s level in saliva.
- There is a suggestion that Ph is more critical than Ca in plaque mineralization.
- Early plaque of heavy former àmore Ca ,3 times Ph &less K than non calculus former.